Oncology Patient Education
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Heart Failure
Condition Basics
What is heart failure?
Heart failure means that your heart muscle doesn't pump as much blood as your body needs. Failure doesn't mean that your heart has stopped. It means that your heart isn't pumping as well as it should.
Because your heart cannot pump well, your body tries to make up for it. To do this:
- Your body holds on to salt and water. This increases the amount of blood in your bloodstream.
- Your heart beats faster.
- Your heart might get bigger.
Your body has an amazing ability to make up for heart failure. It may do such a good job that you don't know you have a disease. But at some point, your heart and body will no longer be able to keep up. Then fluid starts to build up in your lungs and other parts of your body.
This fluid buildup is called congestion. It's why some doctors call the disease congestive heart failure.
What causes it?
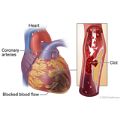
Any problem that damages your heart or affects how well it works can lead to heart failure. This includes coronary artery disease, heart attack, high blood pressure, heart valve problems, and diabetes.
What are the symptoms?
Heart failure symptoms include feeling weak, lightheaded, and very tired. Fluid builds up in your lungs and other parts of your body. This causes you to be short of breath and have swelling in your body.
How is it diagnosed?
Your doctor may diagnose heart failure based on your symptoms and a physical exam. But you will need tests, such as an echocardiogram, to find the cause and type of heart failure so that you can get the right treatment.
How is heart failure treated?
Heart failure is treated with medicines, a heart-healthy lifestyle, and the steps you take to check your symptoms. Treatment may also include a heart device, such as a pacemaker. Treatment can slow the disease, help you feel better, and help keep you out of the hospital. Treatment may also help you live longer.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Any problem that damages your heart or affects how well it works can lead to heart failure. The following lists are examples of these problems.
Problems that damage the heart muscle
- High blood pressure
- Heart attack
- Coronary artery disease
- Diabetes
- Alcohol and illegal drugs (such as cocaine)
- Some prescription medicines (such as those for chemotherapy)
- Heart problems you've had from birth (congenital heart disease)
- Infection or inflammation of the heart muscle (such as myocarditis)
Things that damage the heart's valves
- Valve problems you've had since birth
- Infection of a heart valve (endocarditis)
- Rheumatic fever
Problems with the heart's electrical system
- Fast, slow, or irregular heart rhythms, including atrial fibrillation
- Electrical signals that don't flow as they should from the upper to the lower part of the heart (heart block)
Other problems
- Disease of the sac around the heart (pericarditis)
- Postpartum cardiomyopathy (a rare problem that can happen late in a woman's pregnancy or within the first 5 months after delivery)
- Severe anemia
- Hyperthyroidism
Learn more
What Increases Your Risk
Your risk of having heart failure is higher if you have certain risk factors. A risk factor is anything that increases your chance of having a certain problem.
Heart failure is usually caused by another health problem. So anything that increases your risk for one of those problems also increases your risk for heart failure. These problems include:
- Coronary artery disease and heart attack. Risk factors include smoking, having high cholesterol or diabetes, and having a family history of heart disease.
- High blood pressure. Risk factors include being overweight, being inactive, and having a family history of high blood pressure.
- Heart valve disease. Risk factors include older age and an infection of the valves.
Your risk of heart failure also rises as you get older.
Learn more
Prevention
The best ways to help prevent heart failure are to have a heart-healthy lifestyle and manage existing health problems like high blood pressure and diabetes.
To reduce your risk for heart failure:
- Don't smoke.
If you smoke, quit. Avoid secondhand smoke too. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- Eat heart-healthy foods.
Eat fruits, vegetables, fish, lean meats, and whole grains. Choose foods that are low in saturated fat, and avoid trans fat. Limit sodium, alcohol, and sugar.
- Be active.
Try to do activities that raise your heart rate. Aim for at least 2½ hours of moderate exercise a week. Walking is a good choice. You also may want to do other activities, such as running, swimming, cycling, or playing tennis or team sports.
- Stay at a healthy weight.
Being active and eating healthy foods can help you stay at a healthy weight or lose weight if you need to.
- Manage other health problems.
Many health conditions can raise your risk for heart failure. These include heart attack, high blood pressure, and diabetes. You can help manage many health problems and stay as healthy as possible with a heart-healthy lifestyle and medicines. If you think you may have a problem with alcohol or drug use, talk to your doctor. Your doctor can help you figure out what type of treatment is best for you.
Learn more
Symptoms
Symptoms of heart failure start to happen when your heart can't pump enough blood to the rest of your body.
In the early stages of heart failure, you may:
- Feel tired easily.
- Be short of breath when you exert yourself.
- Feel like your heart is pounding or racing (palpitations).
- Feel weak or dizzy.
As heart failure gets worse, fluid starts to build up in your lungs and other parts of your body. This may cause you to:
- Feel short of breath even at rest.
- Have swelling (edema), especially in your legs, ankles, and feet.
- Gain weight. This may happen over just a day or two, or more slowly.
- Cough or wheeze, especially when you lie down.
- Feel bloated or sick to your stomach.
Sudden heart failure and its symptoms
Sudden heart failure occurs when heart failure symptoms get worse very quickly. Your heart suddenly cannot pump as much blood as your body needs. Sudden heart failure is an emergency. You need care right away.
When you have sudden heart failure, you may have severe trouble breathing. You may cough up pink, foamy mucus. And your heart may start to beat very fast or with an uneven rhythm.
Classifying heart failure based on your symptoms
The New York Heart Association has classified heart failure by how bad symptoms are when you are active.footnote 1 The four classes range from having few or no symptoms when active to having symptoms even when at rest.
- Class I.
People whose physical activity is not limited. Ordinary physical activity does not cause tiredness (fatigue), heart palpitations, trouble breathing, or chest pain. Ordinary physical activity includes activities like house cleaning, short walks, and gardening.
- Class II.
People who have some limitation on physical activity. They are comfortable at rest, but ordinary physical activity causes fatigue, heart palpitations, trouble breathing, or chest pain.
- Class III.
People who have a marked limitation on physical activity. They are comfortable at rest, but less-than-ordinary physical activity causes fatigue, heart palpitations, trouble breathing, or chest pain.
- Class IV.
People who are unable to carry on any physical activity without symptoms. Symptoms may be present even at rest.
Learn more
What Happens
Heart failure is a lifelong (chronic) disease.
Treatment may be able to slow the disease and help you feel better. But heart failure tends to get worse over time. Despite this, there are many steps you can take to feel better and stay healthy longer.
Early on, your symptoms may not be too bad. As heart failure gets worse, symptoms typically get worse, and you may need to limit your activities. Heart failure can also get worse suddenly. If this happens, you need emergency care. Then, after treatment, your symptoms may go back to being stable (which means they stay the same) for a long time.
Heart failure can lead to other health problems, such as heart rhythm problems. Over time, your treatment options may change, especially as your symptoms get worse. You may want to think about what kind of care you want at the end of your life.
Stages of heart failure
Heart failure stages are based on how it often progresses. Stage A means that a person is at risk for heart failure. In stage B, there are signs that the heart is not normal. Stage C means that a person has heart failure with symptoms. In stage D, a person has severe heart failure. footnote 2
Learn more
When to Call a Doctor
Call 911 or other emergency services immediately if you have:
- Symptoms of sudden heart failure, such as:
- Severe shortness of breath (trouble getting a breath even when resting).
- Suddenly getting an irregular heartbeat that lasts for a while, or getting a very fast heartbeat along with dizziness, nausea, or fainting.
- Foamy, pink mucus with a cough and shortness of breath.
- Symptoms of a heart attack, such as:
- Chest pain or pressure, or a strange feeling in the chest.
- Sweating.
- Shortness of breath.
- Nausea or vomiting.
- Pain, pressure, or a strange feeling in the back, neck, jaw, or upper belly, or in one or both shoulders or arms.
- Lightheadedness or sudden weakness.
- A fast or irregular heartbeat.
- Symptoms of a stroke. These include:
- Sudden numbness, tingling, weakness, or paralysis in your face, arm, or leg, especially on only one side of your body.
- Sudden vision changes.
- Sudden trouble speaking.
- Sudden confusion or trouble understanding simple statements.
- Sudden problems with walking or balance.
- A sudden, severe headache that is different from past headaches.
Call your doctor now if you have a pacemaker or ICD and think you have an infection near the device. Signs of an infection include:
- Changes in the skin around your pacemaker or ICD, such as:
- Swelling.
- Warmth.
- Redness.
- Pain.
- Fever not caused by the flu or another illness.
Call your doctor soon if you have symptoms of heart failure, which include:
- Being very tired or having weakness that prevents you from doing your usual activities.
- Having breathing problems such as:
- Trouble breathing during routine activities or exercise that did not cause problems before.
- Sudden shortness of breath, even if it is mild.
- Shortness of breath when you lie down.
- Waking up at night with shortness of breath or feeling as though you are suffocating.
- A dry, hacking cough, especially when you lie down.
- Sudden weight gain, such as more than 2 lb (0.9 kg) to 3 lb (1.4 kg) in a day or 5 lb (2.3 kg) in a week. (Your doctor may suggest a different range of weight gain.)
- Increased fluid buildup in your body (most often in the legs).
Call your doctor soon if:
- Your heart failure symptoms get worse.
- You have a sudden change in symptoms.
- You're having trouble keeping even minor symptoms under control.
Exams and Tests
To diagnose heart failure, your doctor will:
- Ask about your medical history.
Your doctor will also review all the medicines you take, ask if you have heart disease in your family, and look for other risk factors, such as high blood pressure.
- Do a physical exam.
Your doctor will check your blood pressure and heart rate, check your weight, listen to your lung and heart sounds, check your belly and legs for swelling, and look for swelling or bulging veins in your neck.
Your doctor may diagnose heart failure from your symptoms and the physical exam. But you will have more tests to find the cause and type of heart failure so that you can get the right treatment. Tests can show how well your left lower heart chamber (left ventricle) and the valves inside your heart are working. Common tests include:
- Blood tests.
- Routine blood tests can help your doctor identify the cause of heart failure, find out if your kidneys and liver have been affected, and know whether you have risk factors, such as diabetes.
- A brain natriuretic peptide (BNP) test can help diagnose heart failure by checking the amount of a certain hormone in your blood.
- Electrocardiogram (EKG or ECG).
An EKG is done to find any problems with your heart rhythm. It can also show signs of damage to the heart.
- Chest X-ray.
A chest X-ray gives your doctor a picture of your heart, lungs, and major blood vessels.
- Echocardiogram (echo).
This is an ultrasound exam of the heart. An echo can help show whether you have heart failure, what type it is, and what might be causing it.
Your doctor may order more imaging tests. These include:
- Cardiac blood pool scan.
This test shows how well your heart pumps blood to the rest of your body.
- Magnetic resonance imaging (MRI).
An MRI lets your doctor see the structure of your heart and check how well it is pumping.
Learn more
Treatment Overview
Heart failure is treated with medicines, a heart-healthy lifestyle, and doing things to care for yourself at home. Treatment may also include a heart device, such as a pacemaker. You and your doctor can work together to find the best treatment.
Your treatment also depends on:
- The cause of your heart failure.
- Which type of heart failure you have.
- How bad your symptoms are.
- Your goals, wishes, and preferences about your treatment.
As part of your ongoing treatment, your doctor will also try to prevent or treat problems—such as arrhythmia and anemia—that can lead to sudden heart failure.
Sometimes heart failure can be fixed if another problem can be corrected, such as hyperthyroidism. But this isn't common.
Treatment can slow the disease, help you feel better, and help keep you out of the hospital. Treatment may also help you live longer.
- You'll probably take several medicines. Medicines don't cure heart failure. But they can help control symptoms and help you stay healthier longer. And they may help your heart work better.
- You'll take steps to care for yourself at home.
- You'll watch for changes in your symptoms. For example, it's important to watch for sudden changes in your weight. A sudden weight gain can mean that more fluid is building up and your heart failure is getting worse.
- You will follow a heart-healthy lifestyle, which includes limiting sodium, getting regular exercise, not smoking, and eating healthy foods.
- You might attend cardiac rehabilitation (rehab) to get education and support that help you make lifestyle changes and stay as healthy as you can.
- You may get a heart device. A pacemaker helps your heart pump blood better. An implantable cardioverter-defibrillator (ICD) can stop abnormal heart rhythms. A ventricular assist device (VAD), also known as a heart pump, helps the heart pump more blood.
- A heart transplant may be an option for some people with heart failure. During this surgery, a doctor removes a diseased heart and replaces it with a donor heart. Transplants aren't common.
- If your symptoms are severe even though you're getting treatment, you may choose palliative care to help improve your quality of life.
- As with any chronic disease, you can plan ahead for what kind of care you want if you become very ill. This is called advance care planning.
Learn more
Self-Care
Medicines
- Be safe with medicines. Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
- You will get more details on the specific medicines your doctor prescribes. Medicines can help your heart work better, help you feel better, and help keep you out of the hospital. Medicines may also help you live longer.
- Talk with your doctor or pharmacist before you take a new prescription or over-the-counter medicine. Ask if the medicine is safe for you to take. Some medicines can affect your heart and make heart failure worse. Others may keep your heart failure medicines from working right. Over-the-counter medicines that you may need to avoid include herbal supplements, vitamins, pain relievers called NSAIDs, antacids, laxatives, and cough, cold, flu, or sinus medicine.
Diet
- Eat heart-healthy foods. These foods include vegetables, fruits, nuts, beans, lean meat, fish, and whole grains.
- Your doctor may suggest that you limit sodium. Your doctor can tell you how much sodium is right for you. An example is less than 3,000 mg a day. This includes all the salt you eat in cooking or in packaged foods. People get most of their sodium from processed foods. Fast food and restaurant meals also tend to be very high in sodium.
- Limit your fluid intake if your doctor tells you to. Your doctor will tell you how much fluid you can have in a day.
Symptoms
- Weigh yourself without clothing at the same time each day. Record your weight. Call your doctor if you have a sudden weight gain, such as more than 2 to 3 pounds in a day or 5 pounds in a week. (Your doctor may suggest a different range of weight gain.) A sudden weight gain may mean that your heart failure is getting worse.
- Check your symptoms every day to watch for changes. Know what to do if your symptoms get worse.
Activity
- Be active. Do not start to exercise until you have talked with your doctor. Together you can make an exercise program that is enjoyable and safe for you. Regular exercise can make your heart and your body stronger. Being active can help you feel better too.
- With your doctor, plan how often, how long, and how hard you will be active. Don't exercise too hard because it can put stress on your heart.
- If your doctor has not set you up with a cardiac rehabilitation (rehab) program, ask if it's right for you. Cardiac rehab can give you education and support that help you stay as healthy as possible.
- When you exercise, watch for signs that your heart is working too hard. You are pushing yourself too hard if you cannot talk while you are exercising. If you become short of breath or dizzy or have chest pain, stop, sit down, and rest.
Heart-healthy lifestyle
- Do not smoke. Smoking can make a heart condition worse. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good. Quitting smoking may be the most important step you can take to protect your heart.
- Stay at a healthy weight. Lose weight if you need to.
- Manage other health problems such as diabetes and high blood pressure.
- Limit or avoid alcohol. Ask your doctor how much alcohol, if any, is safe for you.
- If you think you may have a problem with alcohol or drug use, talk to your doctor.
- Avoid infections such as COVID-19, colds, and the flu. Get the flu vaccine every year. Get a pneumococcal vaccine shot. If you have had one before, ask your doctor whether you need another dose. Stay up to date on your COVID-19 vaccines.
Learn more
- Conserving Your Energy
- Healthy Eating: Eating Less Sodium
- Heart Failure: Activity and Exercise
- Heart Failure and Sexual Activity
- Heart Failure: Checking Your Weight
- Heart Failure Daily Action Plan
- Heart Failure: Tips for Easier Breathing
- Heart Failure: Track Your Weight, Food, and Sodium
- Heart Failure: Watching Your Fluids
- Immunizations
Medicines
Medicines can help your heart work better, help you feel better, and help keep you out of the hospital. Medicines may also help you live longer.
It's very important to take your medicines exactly as your doctor says.
Medicines include:
- ACE (angiotensin-converting enzyme) inhibitors. These relax and widen blood vessels. This makes it easier for blood to flow through the vessels.
- Aldosterone receptor antagonists. These are a type of diuretic. They make the kidneys get rid of extra fluid and lower blood pressure. They also help keep the heart muscle healthy.
- ARBs (angiotensin II receptor blockers). These relax and widen blood vessels. This makes it easier for blood to flow through the vessels.
- ARNI (angiotensin receptor neprilysin inhibitor) medicine. These make it easier for blood to flow through the vessels.
- Beta-blockers. These slow the heart rate. They also lower the workload on the heart.
- Diuretics. These reduce swelling. They do this by helping the kidneys get rid of excess fluid. They also help prevent fluid buildup in the lungs.
- Hydralazine. This is taken with a nitrate to widen blood vessels. It can lower blood pressure and reduce the workload on the heart.
- SGLT2 inhibitors. These help the kidneys get rid of excess fluid and sodium. They may widen the blood vessels and reduce the workload on the heart.
The medicines you take will depend on the type of heart failure you have.
Supplements, vitamins, and hormones
You may hear that people use supplements, vitamins, or hormones, and that these products might help heart failure symptoms. But there is not much evidence that they help.
Fish oil (omega-3 fatty acid) supplements may help some people who have heart failure. Fish oil supplements, taken along with heart failure medicines, may help people stay out of the hospital and live longer.footnote 2
No other supplement, vitamin, or hormone has been proven to relieve heart failure or help you live longer.footnote 2
Talk to your doctor before you take any over-the-counter medicine or supplement. They may be used along with medical treatments for heart failure, not instead of treatment.
Learn more
Coping With Your Feelings
Emotions such as worry, sadness, or fear can be a normal part of living with heart failure. It's okay if the feelings come and go. But sometimes feelings like anxiety or depression can hang on. They can keep you from doing things to take care of your heart, like limiting salt and weighing yourself. And not doing these things may send you to the hospital.
Having healthy emotions can help you live better with heart failure. That's why your doctor may ask you about your feelings. Or maybe you and your doctor haven't talked yet about how your emotions can affect your heart. It's okay for you to bring it up with your doctor. Working together, you and your doctor can find ways to help you and your heart feel better.
Talking to your doctor about your feelings
Your emotions affect your physical health, so your doctor needs to hear about how you're feeling. Feelings, especially negative ones like anxiety or depression, may be hard to talk about. But your doctor can help with your emotional health just like they have been treating your heart failure. The sooner you talk to your doctor about your emotions and your options for treatment, the sooner you can start to feel better.
Here are some ideas that can help you get ready to talk to your doctor.
- Think about your emotions.
Take some time to think about how you're feeling. Try to picture how you deal with emotions in your daily life.
If you find it hard to think about emotions, that's okay. You could ask someone you trust and who knows you well to let you know what they may notice. Sometimes hearing another person's view can give you new insight.
- Write about your emotions.
It may help you to write about your feelings. To get started, try asking yourself the following questions. Write down your answers and share them with your doctor. Having specific examples will help your doctor have a better idea of how to help you.
- What emotions are bothering me? (Examples: nervousness, worry, sadness, anger, or fear)
- When are these feelings worse? Who or what makes me feel that way?
- When do I feel a little bit better? What people and situations help make me feel okay?
- Am I having trouble sleeping?
- Am I having trouble concentrating?
- How long have I felt this way?
- Is there anything else I think my doctor should know?
Getting support
Emotional support from friends and family can help you cope with the struggles of heart failure. But it can be hard to ask for the help and support you want or need. Remember that people may want to help, but they may not know how. Sometimes it is up to you to ask. Support can make the difference between a good day and a bad day.
Professionals and rehab
Your doctors, nurses, and other health professionals can give you support. And a cardiac rehabilitation program also offers support for you and your family.
Support groups
Support can also come from others who are dealing with the same things you are. Support groups can show you that you're not alone with your feelings or frustrations. They may even give you new ideas to help you cope or solve a problem. You may find that a heart failure support group helps you talk about what's going on in your life.
Your doctor may be able to tell you about the types of support and support groups that are available where you live.
Learn more
Related Information
References
Citations
- Heidenreich PA, et al. (2022). 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association. Journal of the American College of Cardiology, published online April 1, 2022. DOI: 10.1016/j.jacc.2021.12.012. Accessed April 1, 2022.
- Heidenreich PA, et al. (2022). 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association. Journal of the American College of Cardiology, published online April 1, 2022. DOI: 10.1016/j.jacc.2021.12.012. Accessed April 1, 2022.
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024 Ignite Healthwise, LLC. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.