Oncology Patient Education
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Femoral-Tibial Bypass Surgery
Surgery Overview
Femoral-tibial bypass is a type of surgery. It redirects blood around narrowed or blocked blood vessels in your lower leg or foot. It may be done if blood flow is severely limited.
Your doctor will use something called a graft to make the blood go around (bypass) the blocked part of your blood vessel. Often the graft is a vein taken from another place in your leg. But sometimes it is a human-made graft. The graft will carry blood from the femoral artery in your groin to the tibial artery in your lower leg or foot.
You will be asleep during the surgery. Or you will get medicine to numb your lower body and prevent pain. The doctor will make cuts in your skin above and below the narrowed or blocked blood vessel. These cuts are called incisions. If one of your veins is being used for the graft, the doctor will make another incision in your leg to take out the vein.
Then the doctor will attach one end of the graft to the femoral artery and the other end to the tibial artery. After the graft is in place and blood is flowing through it, the doctor will use stitches or staples to close the incisions. You will have scars, but they will fade with time.
You may stay in the hospital for at least 2 days. It may take 6 to 12 weeks to fully recover.
How It Is Done
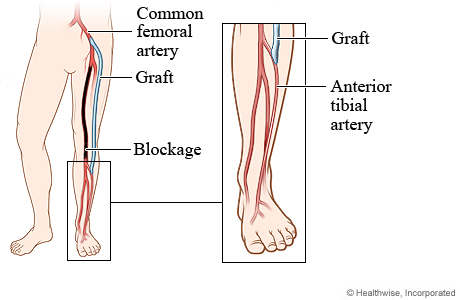
A femoral-tibial bypass is used to bypass a narrowed or blocked artery in the leg. The bypass improves blood flow to the lower leg and foot.
To bypass a narrowed or blocked artery, blood is redirected through a graft. The graft is either a healthy blood vessel that has been transplanted or a human-made material. This graft is sewn above and below the diseased artery so that blood flows through the graft and around the diseased part.
In this picture, a graft bypasses a blockage in an artery near the knee. The graft connects the common femoral artery near the hip to a tibial artery in the lower leg.
What To Expect
You may stay in the hospital for at least 2 days.
You will have some pain from the cuts (incisions) the doctor made. This usually gets better after about 1 week. You can expect your leg to be swollen at first. This is a normal part of recovery. It may last 2 or 3 months.
You will need to take it easy for at least 2 to 6 weeks at home. It may take 6 to 12 weeks to fully recover.
You may need to take at least 2 to 6 weeks off from work. It depends on the type of work you do and how you feel.
You will have regular tests to check for problems with the graft.
Why It Is Done
This surgery is done for people who have narrowed or blocked tibial or peroneal arteries, which are in the leg. Usually, a person has severe symptoms or the problem is limb-threatening before bypass surgery is considered.
Learn more
How Well It Works
Femoral-tibial bypass surgery can improve blood flow when blood vessels are very narrow or blocked.footnote 1, footnote 2, footnote 3
Risks
All surgeries carry a certain amount of risk. These risks include:
- Infection.
- Bleeding.
- Heart attack or stroke.
Specific risks for this bypass surgery include:
- Leg swelling.
- Failed or blocked grafts.
References
Citations
- Conte MS, et al. (2019). Global vascular guidelines on the management of chronic limb-threatening ischemia. Journal of Vascular Surgery, 69(6S): 3S–125S.e40. DOI: 10.1016/j.jvs.2019.02.016. Accessed June 1, 2023.
- Gerhard-Herman MD, et al. (2016). 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease. Circulation, published online November 13, 2016. DOI: 10.1161/CIR.0000000000000471. Accessed November 25, 2016.
- Conte M, et al. (2015). Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: Management of asymptomatic disease and claudication. Journal of Vascular Surgery, 61(3S): 2S–41S. DOI: 10.1016/j.jvs.2014.12.009. Accessed November 25, 2016.
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024 Ignite Healthwise, LLC. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Ignite Healthwise, LLC.




